The Case:
Q. Is this patient having an acute myocardial infarction?
Educational Objectives:
2. Integrate critical assessment strategies to better identify ischemia superimposed on LBBB
3. Incorporate into practice a decision rule to avoid missing acute myocardial infarction masked by LBBB.
Clinical Bottom Line:
A Sgarbossa score of 3 or greater is useful to diagnose an acute myocardial infarction in the presence of LBBB.
The Case:
A 45-year-old male lawyer presents with a 1-hour history of substernal chest pain. He has a history of GERD and hypertension. He is diaphoretic and SOB. On examination, his BP is 118/86, pulse is 86 regular and the rest of the examination is unremarkable. Appropriate lab investigations have been sent and his ECG reveals a LBBB pattern.
Q. Is this patient having an acute myocardial infarction?
The Question:
In the presence of LBBB, can specific ECG criteria aid clinicians in determining if this patient is having an acute myocardial infarction?
The Study:
Electrocardiographic Criteria for Detecting Acute Myocardial Infarction in Patients With Left Bundle Branch Block: A Meta-analysis.
Tabas, J. A., et al, Ann of Emerg Med, Oct 2008, Vol 52, No. 4, pages 329-336
Background:
Prior to the age of revascularization, the issue of identifying an acute myocardial infarction in the presence of left bundle branch block was largely academic. Since the advent of “clot busters” and PCI, this distinction has taken on greater urgency. Approximately 1 to 5% of patients with symptoms of acute myocardial infarction have a LBBB on initial ECG and 30-50% will have a confirmed MI. Among all AMI 7% will have a LBBB. LBBB MI patients often fail to receive timely, guideline-directed care and have higher baseline mortality. The NNT for AMI with LBBB is 21 (95% CI 12 to 72), higher than patients with anterior MI (NNT=28). Furthermore, ACEP guidelines rate “any type of BBB (right, left, and atypical – new or old) thought to be obscuring ST-segment analysis in patients with clinical presentation strongly suggestive of AMI” as a level A recommendation (high degree of clinical certainty based on evidence) for revascularization treatment.
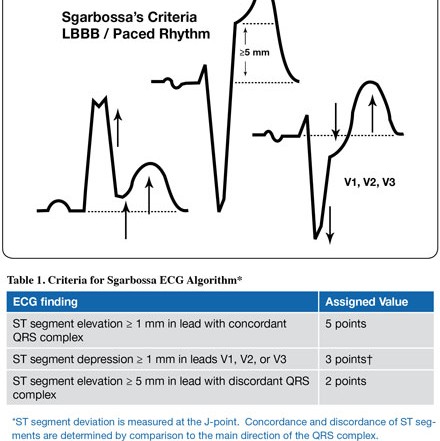
In LBBB, the ST segments are discordant (deviated in the opposite direction) to the major direction of the QRS complex, making the diagnosis of AMI difficult contributing to delays in revascularization. Sgarbossa derived a scoring system for predicting AMI in the presence of LBBB by comparing patients with LBBB in the GUSTO-1 database to an outpatient ECG database (see Table 1). A score of 3 or greater had a positive likelihood ratio of 7.8 and negative LR of 0.2 for the presence of AMI. Since then, the Sgarbossa criteria have met with conflicting reports regarding diagnostic accuracy and clinical usefulness in suspected AMI. The current article attempts to clarify these criteria through the use of a systematic review.

The authors identified ten studies with 1,614 patients with a Sgarbossa score of greater than or equal to 3. The positive likelihood ratio was 7.9 (95% CI 4.5 to 13.8) and a negative LR of 0.8 (95% CI 0.8 to 0.9). In seven studies with 1,213 patients with a Sgarbossa score of greater than or equal to 2, positive LR was 0.7 to 6.6 and negative LR was 0.2 to 1.1. There was significant intra- and interobserver agreement.
The ECG shows concordant ST segment elevation of 1 mm in leads V4 and V5 for a Sgarbossa score of 5. The patient underwent urgent cardiac catheterization with stenting and made an uneventful recovery.
A Sgarbossa score of 3 or more is useful to rule in a diagnosis of an acute myocardial infarction in the presence of LBBB on the ECG. This represents concordant ST elevation of greater than or equal to 1mm or ST depression of greater than or equal to 1mm in leads V1 to V3. A score of 2, which equates to 5mm of ST deviation, was not helpful in diagnosing acute myocardial infarction.
Comment
Although the authors have shown the utility of the Sgarbossa criteria to rule in a diagnosis of AMI with LBBB, its clinical utility may be limited. Kontos and Li demonstrated that only 3% of 372 patients with LBBB and suspected ischemia met the Sgarbossa criteria. Using decision analysis, Shiplap concluded that if reperfusion therapy were used for all LBBB patients with suspected AMI then 10 additional stroke free lives would be saved per 1000 patients compared to a strategy using the Sgarbossa criteria to more selectively suspected AMI in LBBB subjects. In trying to resolve which LBBB with suspected AMI to reperfuse, the best strategy may be to treat all of them regardless of ECG criteria.