Oils on the black pavement are freshly released as the cool rain drizzles upon it. Typical morning rush hour traffic as drivers vie for position. She slams on her brakes to avoid a passing car. At 55 mph, her sedan spins out of control. Miraculously avoiding other vehicles, the sedan comes to a stop by sideswiping the median. The driver, Mary S., unbuckles her restraints and runs from the vehicle. One case presentation. Two distinct courses of action. You judge which is right.
One case presentation. Two distinct courses of action. You judge which is right.
Oils on the black pavement are freshly released as the cool rain drizzles upon it. Typical morning rush hour traffic as drivers vie for position. She slams on her brakes to avoid a passing car. At 55 mph, her sedan spins out of control. Miraculously avoiding other vehicles, the sedan comes to a stop by sideswiping the median. The driver, Mary S., unbuckles her restraints and runs from the vehicle.
EMS arrives to find Mary sitting on the median crying. Her vehicle is facing backwards on the highway. The passenger side is scraped and against the median. A large dent exists on the passenger side front bumper. All glass is intact.
Reluctantly, Mary is spider strapped to a backboard and C-collar applied. The sleeves to her leather coat are cut and bilateral 18 gauge IVs are inserted. The medic calls in report; “We have a 48-year-old female victim of a highway speed MVC. Fully restrained, airbags deployed. Victim hysterical at scene. Unsure of LOC, victim can’t describe accident. Hurts all over. Vitals 118/70, 98, 16. Sa02 100 on NRB. PMH hypertension. Allergies penicillin. Meds lisinopril. LMP 6 months ago. ETA 10 minutes.”
Level 2 trauma activation is paged at the receiving facility. The trauma team is anxiously waiting at the door.
Below we present the exact same case to two doctors with equivalent training, Drs. Patel and Dr. Silva.
***********************
Scenario 1: Dr. Patel
As physician in charge, Patel states, “This sounds bad. Spike the bags, load the rapid infuser, open the vascular access and chest tube trays. Keep the CT suite empty and waiting.”
EMS rolls in. Mary is hastily lifted onto the hospital gurney. Her clothes are completely cut off and full monitoring is applied. The IVs are replaced with ‘sterile’ hospital IVs. Mary screams,” Get this thing off my neck, it hurts! I can’t breathe with this mask over my face!”
Patel introduces himself. Tears are painting Mary’s cheeks with mascara. “The collar is to keep you from being paralyzed if you have a fractured neck. The mask is helping you breath.” Patel looks up at the monitor. Heart rate increased to 105. Patel thinks; tachycardia, internal injuries, hysterical, altered LOC.
Mary is logrolled, no step offs, generalized tenderness, rectal tone good, guaiac negative. Rest of the exam reveals mild tachycardia, generalized tenderness to right knee and ankle without bruising or swelling, mild erythema to skin over left clavicle. Head to toe exam is otherwise normal. FAST exam is negative. Portable CXR is normal.
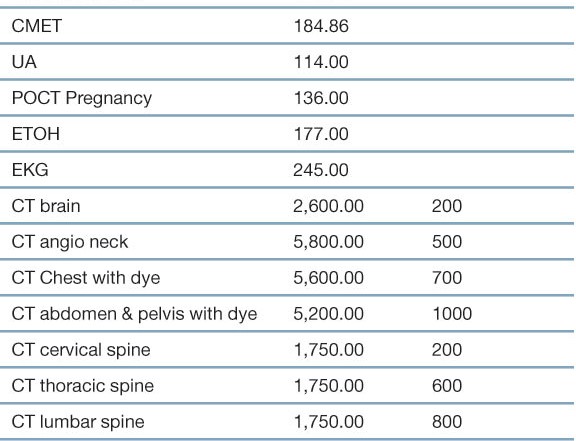
Patel decides due to highway mechanism he will pan scan Mary. A CT with IV dye is ordered of the chest, abdomen and pelvis. CTs with recons of the cervical, thoracic and lumbar spine are ordered. Patel is well educated. He takes no chances. CT of the brain is ordered. X-ray everything that hurts. Plain films of the right femur, knee, tib/fib and ankle are ordered. Mary works for a law firm, you never know. Worried about a vascular injury due to the clavicle erythema a CT angio of the neck is ordered. Patel prepares Mary for potential surgery. CBC with differential, PT/PTT, CMP (Patel wants to check for liver damage), urinalysis, HCG, urine toxicology, ETOH and EKG are ordered. Two units of PRBC are crossed and held for Mary.
*********************
Scenario 2: Dr. Silva
Silva is waiting at the door with his team. He tells the team not to open any kits or trays. EMS did not report any significant injuries and vitals were normal. He is aware of a patient needing a CT and tells radiology not to hold the suite open.
As Mary is being lifted to the gurney, Silva asks the medics about glass breakage, deformity of the vehicle body, if any other vehicles were involved and if anyone else was hurt. The medics answer no to all.
Mary is sobbing. Silva takes the NRB mask off. He wants to see what her Sa02 is on room air. It remains at 100. He asks Mary if she was knocked out and if she remembers the accident. Mary states, “I don’t know, it all happened so fast. I have no idea where that car came from. I remember spinning around, hearing my car hit the wall. I thought the car was on fire and got away as fast as I could.” Good detailed story, Silva thought.
As the nurses start to replace the IVs and cut off Mary’s clothes, Silva tells them to stop, ‘hopefully the IVs won’t be in for long and let me examine her first.’
Silva opens her clothes and listens to her heart, lungs and abdomen, he palpates firmly. Except for mild tachycardia and erythema on her left clavicle all is normal. Seat belts did what they’re supposed to do.
Silva then proceeds to the HEENT exam. Mild generalized stiffness in the upper traps bilaterally, otherwise normal. Using Nexus Criteria, Canadian C-spine rules and GLASS Criteria, Silva removes the c-collar and clears the cervical spine. Mary is log rolled, her back exam reveals mild generalized paraspinal tenderness, and no step offs or point tenderness. Clothes are completely removed as Mary is rolled. Silva does a complete head to toe exam. Mild generalized tenderness to right knee and ankle. No bruising or swelling. Ottawa ankle and knee rules as well as FABER test is all negative. Complete passive and active ROM as well as vascular checks are all normal.
Silva deactivates the trauma team. He sits Mary up and hands her a cup of ice water. Heart rate decreases to mid-90s. B/P and Sa02 remain normal. “Keep her on the monitor and vitals q15. I’ll recheck her when her family gets here in about an hour.”
************************
What are the ethical considerations to both Mary and society?
The outcome of Mary is identical in both scenarios. Mary is observed in the ED, then ambulated and sent home.
Physicians live in a complex health care environment in which multiple stakeholders influence everyday clinical decisions. Physicians may not be cognizant of the magnitude these conflicting forces have on their medical decision-making.
Dr. Patel may have seemingly legitimate reasons for his extensive workup albeit emotional and not scientific. Patel works in a level one trauma center, where custom is to pan scan. Customs then become standards of care.
Hospital administration may pressure over-triage of trauma patients to maintain their level one trauma designation and increase reimbursement. Multiple for profit companies earn from over triage. There is no disincentive not to over triage for the hospital or physician. There is great disadvantage to the patient and society. Emotional and physical discomfort, excessive radiation exposure, reactions to IV dye, excessive costs, delayed or no care for other patients and loss of personal property are all real and significant.
There are emotional issues for Patel’s decisions. Patel had already planned to aggressively resuscitate the patient prior to her arrival. Would it be embarrassing to have opened a central line kit and not use it? Could his ego handle admitting he was initially wrong? Most of all, the trepidation of missing an injury, no matter how small, even if it does not affect Mary’s outcome. Is it easier to send a patient through a machine than do a thorough history and physical? Do physicians make decisions to benefit themselves regardless of benefit or detriment to the patient?
Many physicians are paid based on RVUs and patient satisfaction scores. Ordering more tests makes the case more complex increasing the RVUs. Public perception is more tests are better, increasing patient satisfaction. Physicians wrongly perceive that more tests protect them from lawsuits. Have physicians’ self-vested interests superseded that of the patients?
Let’s take a look at Dr. Silva’s medical decision making:
Dr. Silva makes no assumptions and does not anchor onto any information based on a sketchy, adrenaline charged EMS report. Silva continues to open-mindedly gather information from the paramedics and the patient. Mary’s emotional and physical needs are attended to. The NRB and C-collar is removed, IVs are not restarted and clothes are not cut. Evidence-based medicine is used to clear her cervical spine, avoiding imaging. He then does a complete physical and plans for serial reassessments prior to making any further decisions. Silva avoids biases and mythical customs.
Lack of unnecessary testing indicates Silva upholds his professional and fiduciary duty to Mary and society. Held blood, CTs and staff are not kept from other patients. Costs are minimized.
Compassion and respect towards the ‘hysterical, crying female’, provides helpful clinical data and a cooperative and appreciative patient. This interaction does more to reduce the risk of litigation than any tests.
Medical businesses greatly influence a physician’s decisions. Ordering of tests to benefit the business and physician is not only unethical but fraudulent. Physicians have a duty to uphold the health and financial interests of their patients above all other stakeholders including themselves.
See NEXT PAGE for a break-down of the costs – both in dollars and radiation exposure – associated with this case









5 Comments
How about a course of action where the ems provider doesnt even take her in? relatively young healthy women self extracts and no high risk complaints whose vital signs normalize after adrenaline subsides.
How about a course of action where the ems provider doesnt even take her in? relatively young healthy women self extracts and no high risk complaints whose vital signs normalize after adrenaline subsides.
Dr Patel did the right thing; I had a similar patient that was found to have at laparotomy to have a rupture of the retro-peritoneal portion of the 4th part of the duodenum. This is a rare, but fatal injury.
The prices of the labs and xrays are exorbitant. I have had an emergency CT chest with contrast: the cost to the insurance company was less that $3000, who reduced payment to about 40%. A urinalysis charge for $114 is absurd.
The figure of 29,000 cancers from CT scans is without any scientific validity, and has been disputed by the ACR.
The documented number of cancers caused by the Chernobyl nuclear accident is 9. (I have been there and have read the UN reports on the subject)
An interesting article. Dr Silva’s approach is more akin to the Emergency Medicine I practiced in the UK prior to a move to Australia. Here in Australia it seems more like Dr Patel’s approach. Whilst I tend towards Dr Silva’s approach, everybody has a story like Dr Meade’s of the injury that was missed. Our consiciences, employers and patients do not accept misses well.
My question to Dr Meade would be, would the patient with the rupture of the RP portion of D4 have been sent home and this injury missed, or would serial examination have revealed pain and tenderness which would then have resulted in either CT or laparotomy? Not rushing to pan-scan is not the same as hasty disposition out the door.
In response to the second comment by Dr. Meade; I once saw a preacher slap a paralyzed women on the head and she got up and walked. I don’t go around smacking paralyzed people on the head expecting them to walk. When did testimonials replace science?