How to handle the ingestion of rare earth magnets
It’s late winter and flu season has segued seamlessly into gastroenteritis season. Seemingly every other patient that presents to your ED has a combination of the same symptoms – abdominal pain, vomiting, and diarrhea. Right on cue, two new patients arrive with the chief complaint of abdominal pain, a 2.5 year old male and a 16 year old female. You enter the room of the toddler and are immediately concerned. He is febrile, tachycardic, and tachypneic with an overall ill appearance. His dad reports the patient began to complain of abdominal pain earlier in the day followed by multiple episodes of non-bilious emesis. On exam the abdomen is distended and tender with absent bowel sounds. An IV is placed followed by administration of a normal saline bolus. Labs reveal a leukocytosis and a KUB demonstrates air-fluid levels and a string of small, circular, radiopaque FBs in RLQ. While you are dealing with this patient, the senior resident evaluates the adolescent. She initially denies any other complaint, but with her mother out of the room tells you that two hours prior to presentation while attempting to apply a fake tongue piercing, the pieces “snapped together” and startled the patient, causing her to swallow them. She admits that she actually has no abdominal pain, but is here because she heard that another person at her school needed surgery after swallowing a piercing.
Foreign Body Ingestion
Foreign body (FB) ingestion is common in the Pediatric population. In 2013, the American Association of Poison Control Centers documented a total of 103,552 FB ingestions. 87,636 were in patients less than 20 years old, with the vast majority of these (73,366) by children less than five years of age. In contrast to adults, most FB ingestions are accidental and involve items commonly found at home such as coins, toys, jewelry, magnets, and batteries. The AAPC numbers support this: 17,513 out 21,501 of “Toy or Miscellaneous Substance” ingestions were by individuals less than 20 years of age and 14,266 were by individuals less than five years of age.
The standard teaching is that FBs tend to lodge in three locations: first, the thoracic inlet, second, the gastroesophageal junction, third, the level of aortic arch. Foreign bodies that pass through the esophagus and enter the stomach are likely to transit the GI system without complication. Those that remain in the esophagus should be removed promptly and those that remain in the stomach may be retrieved by a gastroenterologist. Once past the pylorus, even large or sharp foreign bodies are typically managed expectantly and only removed surgically if complications arise. However, one of the potential exceptions to this strategy, along with button batteries, is the ingestion of rare earth or neodymium magnets.
Rare Earth Magnets
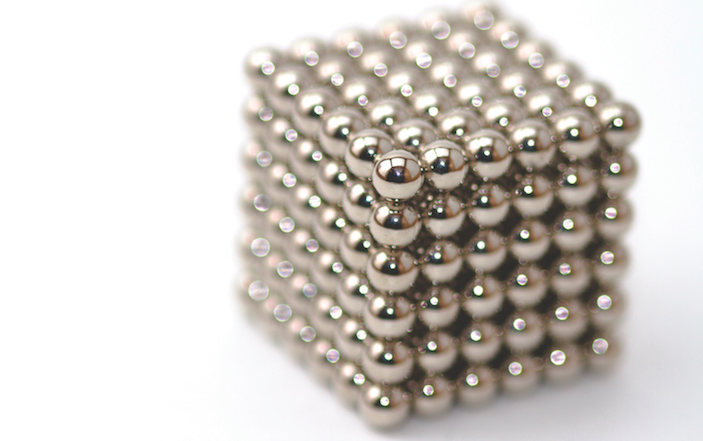
Initially found in building toys for children and then marketed as adult desk toys under such names as “Buckyballs”, “Zen Magnets”, “Neocube”, “Nanodots”, and others, rare earth magnets are sold in sets of hundreds of 3-6mm spheres or cubes. Rare earth magnets consist of alloys of neodymium, iron, boron, or samarium cobalt and are at least 5-10 times stronger than traditional iron magnets. Due to their powerful attractive force, an ingested neodymium magnet is capable of repositioning intestines and finding another magnet or piece of metal through up to 6 layers of bowel wall leading to serious consequences such as ulceration, necrosis, perforation, fistulae, volvulus, obstruction, and peritonitis.
Click on the image to view the Buckyball timeline:

Since the initial report of injury associated with neodymium magnet ingestion in 2002, numerous publications have documented injury and even death associated with multiple magnet ingestion. Data analyzed using the National Electronic Injury Surveillance System database demonstrated an 8.5 fold increase in magnet ingestion from 2002 to 2011, which coincides with the increased availability of rare earth magnets. Interestingly, although the majority of patients reported to have possibly ingested magnets are less than five years of age and male, those thought or known to have ingested rare earth magnets or multiple magnets tended to be older children and adolescents. Adolescent rare earth magnet ingestion is predominantly female which can be explained, in part at least, by the use of these magnets as faux piercings and jewelry.
Compared with other ingested foreign bodies, the majority of which pass spontaneously and require surgical intervention in < 1% of cases, rare earth magnet ingestion is associated with increased morbidity and mortality. Based on preliminary results from a recent survey conducted by the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN) of its membership: 52% of rare earth magnet ingestions resulted in endoscopic intervention alone, 20% with endoscopy and surgery, and 8% resulted in surgery alone. Only 15% were simply observed. Of those who underwent surgery, 41% had repair of a perforation or fistula and 22% required some degree of bowel resection.
Belying the potential seriousness of the problem, presentation of patients with rare earth magnet ingestion may be innocuous. Although some patients may present early after a witnessed or reported ingestion, others may be delayed, as patients are asymptomatic until complications occur. Of those that present with symptoms, they are often described as “flu-like.” Non-bilious emesis is most common, but abdominal pain, abdominal distention, diarrhea, and fever are also reported.
Management of Rare Earth Magnet Ingestion
The first step in diagnosis is to keep the possibility of rare earth magnet ingestion on the differential. In 2012, a detailed algorithm for the management of rare earth magnet ingestion was developed by NASPGHAN.
The initial step for an Emergency Department provider is to obtain an abdominal x-ray to confirm if a magnet is present. If seen on the scout film, then it is imperative to obtain further views to help determine the location of the magnet and presence of a single magnet or multiple magnets (or a single magnet and a metallic FB). This may be tricky as multiple magnets that stick together can overlap and be misinterpreted as a solitary magnet. FBs that appear stacked or slightly separated (possibly by bowel wall) should be regarded as multiple magnets.
Single magnets may be managed as an outpatient with close follow-up and explicit discharge instructions, but strong consideration should be given to consultation with a pediatric gastroenterologist. Multiple magnets (or a single magnet and a metallic FB) should be should be treated with increased urgency. If multiple magnets are suspected, pediatric gastroenterology should be consulted and the patient should be transferred to a facility where pediatric gastroenterology and surgery are available. Due to the increased risk of perforation and fistulae formation, pediatric surgery should definitely be consulted if the ingestion is suspected to have occurred over 12 hours prior to diagnosis (although pressure related injury has been documented as quickly as 8 hours after ingestion).
Pediatric gastroenterology will attempt to remove multiple magnets located in the esophagus or stomach. Symptomatic patients with magnets past the pylorus should be promptly evaluated by pediatric surgery. In asymptomatic patients, pediatric GI may choose to attempt endoscopic or colonoscopic removal; if this is unsuccessful, pediatric surgery may decide on operative intervention. Inpatient observation with serial exams and x-rays (every 4-6 hours initially) is another option. Patients who demonstrate progression of the magnets can be discharged with close follow-up and explicit return precautions. Patients without progression should be reevaluated for endoscopic or surgical removal.
Although there is no published supporting evidence, polyethylene glycol treatment may speed transit of the magnets while also preparing for colonoscopy if the magnets do not pass.
Click on the image to view the flow chart:

Resolution of the Cases
Pediatric surgery and pediatric gastroenterology were consulted to evaluate the 2.5 year old. The patient was taken emergently to the OR and found to have multiple small bowel loops adherent to each other. Multiple magnets were found resulting in pressure necrosis and perforation. Pediatric GI elected to take the adolescent to the OR and removed the magnetic piercing without complication.
REFERENCES
1. Abbas, M. et al. Magnet Ingestions in Children Presenting to US Emergency Departments, 2002–2011. Journal of Pediatric Gastroenterology and Nutrition. 2013; 57(1):18-22.
2. Adikibi, B, et al. Magnetic bead toy ingestion — uses and disuses in children. Pediatric Surgery International. 2013; 29(7):741-744.
3. De Roo, A. et al. Rare-earth magnet ingestion-related injuries among children, 2000-2012. Clinical Pediatrics. 2013; 52(11):1006-1112.
4. Gregori, D. et al. Magnetic FB injuries: An old yet unresolved hazard. International Journal of Pediatric Otorhinolaryngology. 2012; 76(Supplement 1): S42–S48.
5. Hussain, S. et al. Management of Ingested Magnets in Children. Journal of Pediatric Gastroenterology and Nutrition. 2012; 55(3):239-242.
6. Kramer, R. et al. Management of Ingested Foreign Bodies in Children — A Clinical Report of the NASPGHAN Endoscopy Committee. Journal of Pediatric Gastroenterology and Nutrition. 2015: [Epub ahead of print]









1 Comment
My granddaughter is 9. She had 16 in her stomach and one in the small intestine that was being pulled on by the clump in her belly. She has a4inch incision in her chest and two smaller ones where they couldn’t get the scope in. She’ll have the NGtube in for 3 days…iv’s and a catheter due to urinary retention. She is at Doenbecher hops in Portland.